42 yr old female with multiple problems
42 YEAR OLD FEMALE WITH MULTIPLE HEALTH EVENTS"
I have been given this case to solve in an attempt to understand the patient clincal data analysis in order to develop my competency in reading and comprehending clinical data
You can find the original case in the link below-
Following is my analysis on the patient's problem:
MAIN COMPLAINTS:
- Migraine with Aura
- Sleep Disturbances
- Edema mainly confined to face and abdomen
- Increased Pain Tolerance
- Fatigue
- MIGRAINE :
- ONSET: Sudden
- DURATION: Since 2 years of age
- More towards the left side
- Gradually progressive
- ASSOCIATED SYMPTOMS:
- Numbness of left hand and left face felt like someone was pouring ice water over the cheek and also feeling of falling and spinning at night.
- Preceded by AURA associated with transient loss of vision
- Aura starts as a flicker and then eventually becomes a crescent that covers the entire centre of vision
- PAST HISTORY: It was also associated with stuttering and memory loss as well as loss of function of left side and an episode of CSF rhinnorhoea from left nostril.
- RELIEVING FACTOR : Medication (TRIPTANS )
So from the above complaints the possible diagnosis could be :
- HEMIPLEGIC MIGRAINE
- Transient Ischemic Attack (But if she has TIA she is less likely to have other aura symptoms)
- Infections like meningitis, encephalitis (she should have a fever, rash)
- Brain tumours
- Seizures with post-ictal paralysis
- Metabolic Disturbances like Homocystinuria (as she has MTHFR deficiency, she can have high homocysteine levels)
- MELAS ( Mitochondrial Encephalopathy Lactic Acidosis and Stroke like episodes)
In order to confirm the above diagnoses, the possible investigations needed would include:
- CT and MRI of brain can confirm brain tumours, stroke, TIA
- CSF analysis to diagnose infections
- EEG to detect seizures
- Magnetic Resonance Angiography to diagnose TIA
- Intracranial pressure
Possible treatment modalities are :
- Hemiplegic migraine - Triptans (which she is already consuming)
- Surgery (Carotid endareterectomy) - TIA ( cannot give anticoagulants because she has G6PD Deficiency)
- Anti epileptics - Seizures
2. SLEEP DISTURBANCES:
- ONSET: Since birth
- DURATION OF SLEEP: 2-4 hrs and no REM sleep
- POSSIBLE CAUSES:
- G6PD Deficiency impaired the glycolysis so glycine is not formed well . Glycine is also an inhibitory neurotransmitter.
- AMPD1 Deficiency can cause sleep disturbances because Adenosine is an inhibitory neurotransmitter so it should help in sleep.
Treatment taken by her :
- L serine : works like glycine in brain so helps in better sleep
- Cimetidine
3.EDEMA CONFINED TO FACE AMD ABDOMEN:
- ONSET: since 1 year of age
- DURATION: approximately 40 years
- SITE: Face , Abdomen
- AGGRAVATING FACTORS: Emotional Stress , Eating wrong food such as Fava beans , Exercise , Smoke
- RELIEVING FACTORS: Rest
- Associated factors - Shortness of breath, Decreased urination(increased on fasting), Dark coloured urine on exercise
Possible causes for swelling:
- Since she has hemolytic anemia , she could have Right Heart Failure which is responsible for ascites and shortness of breath (because of Pulmonary artery hypertension).
- And the hemolytic anemia could be responsible for her kidney infection because G6PD is responsible for production of NADPH. And since she has deficiency of G6PD, She does not have enough NADPH and ATP which resulted in loss of lots of ions thereby causing decrease in urination and Facial edema. ( refer to edited paragraph -1 )
- It increased on emotional stress and eating fava beans because she has G6PD Deficiency.
- Her shortness of breath could also be attributed to hiatal hernia.
- Dark urine on exercise is suggestive of hemolysis which could be due to G6PD deficiency.
Differential diagnoses :
- Could be Angioedema
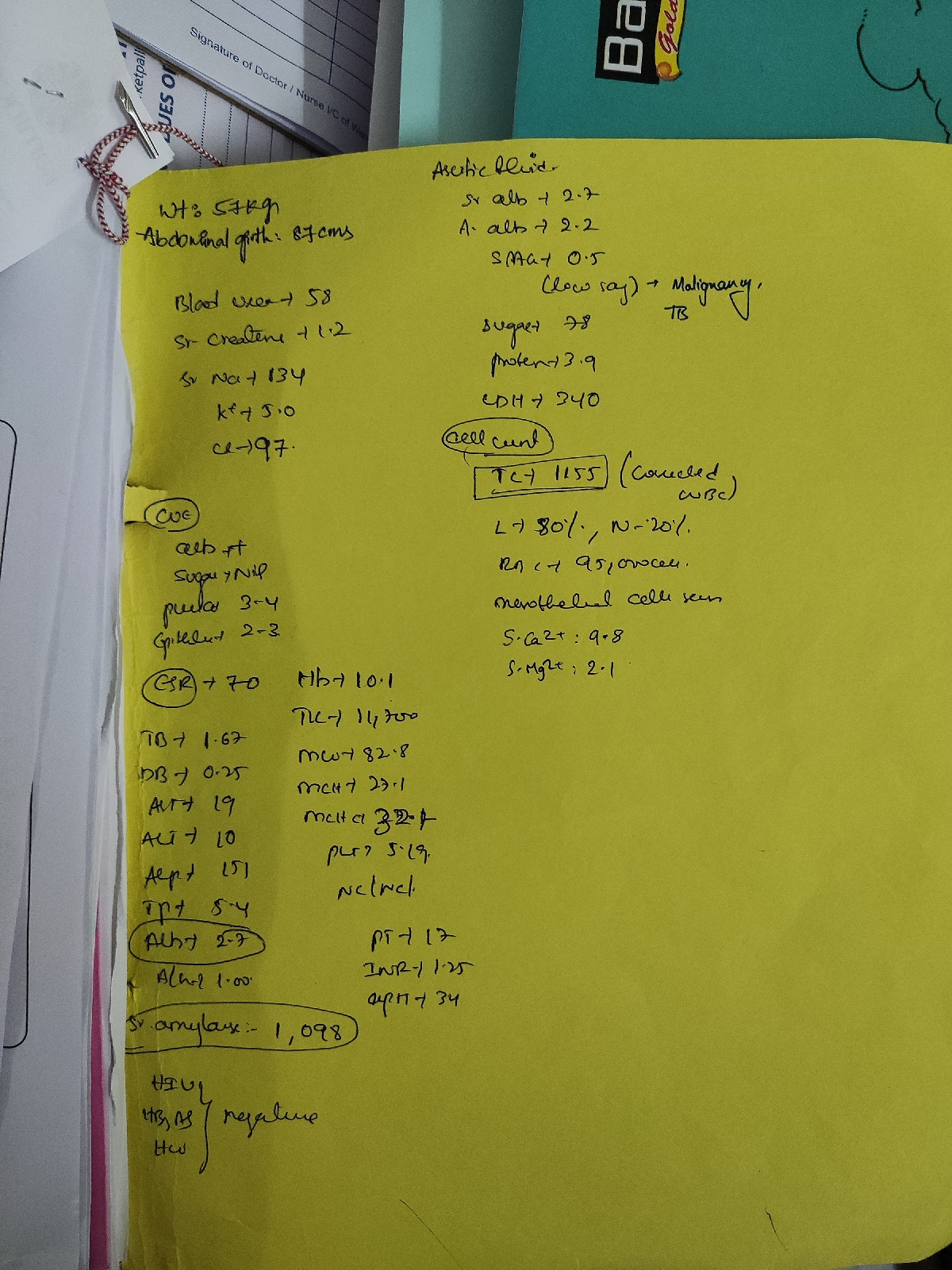
Investigations done in this case are :
- Hemogram - shows anemia
- ECG - signs of Right Heart Failure
- CXR - Left atrial enlargement in this case
- SGPT, SGOT - elevated in this case suggestive of hemolysis
- CUE - to show infection
Further investigations required are :
- LDH -should be elevated To detect hemolysis
- Total BIlirubin - should be elevated
- Reticulocyte count - elevated
- Urobilinogen
- Heinz bodies in RBC on complete blood film
- Beutler fluoroscent spot test - rapid test that identifies NADPH production by G6PD under UV Light
- Haptoglobin ( decreased in hemolysis)
- Direct Coomb's test - negative (suggestive of non autoimmune hemolytic anemia)
- G6PD test
- Skin tests for allergy (for angioedema)
Treatment :
- Avoiding stress
- Do not consume fava beans, sulpha drugs, antimalarials
- Serine- increased urination
- Excess salt consumption
4. INCREASED PAIN TOLERANCE:
- Onset - since 4 years of age, still present
- ASSOCIATED COMPLAINS:
- History of multiple falls
- Fracture of ankle
- PROBABLE DIAGNOSIS:
- Osteoarthritis could be responsible for multiple fractures.
- CIPA (Congenital Intolerance to Pain With Anhydrosis )
Differential Diagnosis:
- CIPA (Congenital Intolerance to Pain With Anhydrosis)
- Osteoarthritis could be responsible for multiple fractures. ( refer to edited paragraph -2 )
Investigations required :
- Genetic testing for CIPA (NTRK 1 gene mutation can cause CIPA)
- X Rays of limbs to diagnose osteoarthritis.
Treatment :
- There is no treatment for CIPA so attention should be given to injuries to prevent infection and worsening injuries.
5. FATIQUE:
- POSSIBLE CAUSES:
- AMPD1 deficiency - lack of ATP hence the person gets easily tired.
- Past history shows parents to be chain smokers which increases the oxidative stress.
- Oxidative stress from excess of free radicals because of G6PD deficiency
- TREATMENT: Ribose - provides ATP.
Other problems of the patient:
- PCOS - Responsible for :
- Dysmenorrhoea
- Ectopic Pregnancy
- Increased Hair loss
- Bipolar disorders, Anxiety, Depression - could be because of less sleep and MTHFR mutation (Methylene Tetrahydrfolate Reductase Deficiency)
- Rashes in face (could be SLE)
- ADHD (Attention Deficit Hyperactivity Disease ) - Because of ANKK 1 mutation.
- VWF mutation (Von Willebrand Factor ) - could be responsible for dysmenorrhoea.
The patient should go for whole genome sequencing to find out the other mutations.
PAST HISTORY IN BRIEF(chronologically):
- At Birth , she had Severe Jaundice
- Tongue tie and upper lip tie
- Large upper tori
- Sleep disturbances(less than 3-4 hrs in a day)
- Edema of face/head and abdomen
- Vomitings, usually watery with salty broth
- Started speaking at 1 1/2 and writing in a language at 2 1/2 itself
- Excessive hair growth on face/neck/toes and legs at 3 years
- Didn't eat properly , i.e., anorexia maybe
- At 4yrs,Chronic UTI, Kidney infections, strep throat, lung infections, multiple sprained ankles and knees
- Severe reaction to Sulfa drugs
- Severe headache(since 2) -Worsens with menses and while on birth control=>MIGRAINE WITH AURA at age 32
- Potential sensory disorder
- Increased pain tolerance
- Severe mood disorder, on trying to calm down it usually precedes a swelling event or migraine
- At 12 , had Cervical degeneration and scoliosis
- At teenage, had anemia
- At 15,attempted suicide as headache worsened and she was bed forced
- Gained enough weight and was about 95lbs at 5'4" and ballooned up and fasted then to lose weight
- At 21,Ectopic pregnancy-she woke up during surgery
- At 22,had chronic abdominal pain and multiple ovarian cysts, diagnosed for PCOS on CT
- At 23,had Severe Kidney Infection and Pneumonia-at this event of hospitalization: Type aB melanoma and 4 precancerous tissues were removed
- At 30 , broke leg while dancing
- At 32, severe reaction to antimalarials-diarrhoea, vomiting, swelling, brain felt like slug. She also got swine flu and pneumonia-was vaccinated for pneumonia then
- At 34 , migraine with aura increased and was associated with transient loss of vision, stuttering, memory loss, left side of face and hand got affected. On lab investigations, poor liver function and mild hemolysis and high post meal cortisol were revealed.
- Anemia was diagnosed as haemolytic----genetic testing showed G6PD AND AMPD1 DEFICIENCY
- At 35, she had failed LASIK surgery and diagnosed of ADHD/Autism spectrum
CURRENT PROBLEMS:
- Frequent falls to left. Left foot started giving out as well as left hand. One fall downstairs broke sprained and broke left ankle
FRACTURE OF ANKLE
- Cravings for large amounts of salt and fats
- Swelling and hair loss
- Fatigue
- Left jaw pain upto face
- Struggle to breath --may be due pulmonary hypertension associated with right heart failure in anemia
- Intolerance to most foods and smoke
- Decreased sweating ( sweats only on emotional stress ,exercise,eating wrong thing, smoke )
- Decreased urination-Dark and yellow colored urinen after stress or exercise--this may be due to hemolysis due to G6PD deficiency.
- Decreased sleep ( nearly no REM ) --due to glycine crisis in AMPD1 and G6PD deficiencies.
Sleep is decreased(nearly no REM)
Edema changes within weeks
CURRENT MEDICATIONS:
- L-Serine 20 mg at night to improve sleep
ON 1st DAY OF L-SERINE
RECENT UPDATES IN THE CASE AS OF MAY,2020 :
Presented with the Complaints of :
1) Oral ulcers
2) Vaginal ulcers
She got diagnosed with Behcets disease.
Possible causes for Behcets : She has multiple mutations making her susceptible to various autoimmune diseases like Behcets.
Symptoms which could be associated with Behcets in this patient are :
1) Headache- Because Behcets is characterised by inflammation within the brain (meningoencephalitis) which can cause a very severe headache associated with poor vision, ataxia, difficulty in speaking.
https://behcets.org.uk/information-for-patients/headache-in-behcets-disease/
2) Poor vision - Behcets is associated with Uveitis. That could be responsible for her poor vision.
3) Personality changes - Sometimes it might be the first symptom which should suggest Behçet’s disease.
Differentials for her complaints could be :
1) Herpes Simplex Labialis
2) Aphthous ulcers
3) SLE (also complains of rash on face)
Investigations required for the above diagnoses are:
1) Mainly based on clinical findings such as oral ulcers, genital ulcers.
2) Skin lesions such as acne, folliculitis, malar rash which are suggestive of SL
3) CSF Analysis which might show lymphocytosis In the case of Herpes Simplex Labialis.
4) CT and MRI may show periventricular white matter atrophy and lesions in the basal ganglia.
5) ESR ( elevated because of inflammation)
6) Complete ocular examination to see uveitis
7) Pathergy test
Treatment modalities : It does not have any treatment. The symptoms can be treated by
i) Topical therapy -
a) Creams for the oral and genital ulcers
b) Eye drops for uveitis
ii) Systemic therapy -
a) Immunosuppressants like Infliximab.
b) High dose corticosteroids.
c) Colchicine can be used for genital ulcers but cannot be used here because of her G6PD deficiency.
iii) Cognitive Behavioural Therapy - which she is undergoing.
Presented with the Complaints of :
1) Oral ulcers
2) Vaginal ulcers
She got diagnosed with Behcets disease.
Possible causes for Behcets : She has multiple mutations making her susceptible to various autoimmune diseases like Behcets.
Symptoms which could be associated with Behcets in this patient are :
1) Headache- Because Behcets is characterised by inflammation within the brain (meningoencephalitis) which can cause a very severe headache associated with poor vision, ataxia, difficulty in speaking.
https://behcets.org.uk/information-for-patients/headache-in-behcets-disease/
2) Poor vision - Behcets is associated with Uveitis. That could be responsible for her poor vision.
3) Personality changes - Sometimes it might be the first symptom which should suggest Behçet’s disease.
Differentials for her complaints could be :
1) Herpes Simplex Labialis
2) Aphthous ulcers
3) SLE (also complains of rash on face)
Investigations required for the above diagnoses are:
1) Mainly based on clinical findings such as oral ulcers, genital ulcers.
2) Skin lesions such as acne, folliculitis, malar rash which are suggestive of SL
3) CSF Analysis which might show lymphocytosis In the case of Herpes Simplex Labialis.
4) CT and MRI may show periventricular white matter atrophy and lesions in the basal ganglia.
5) ESR ( elevated because of inflammation)
6) Complete ocular examination to see uveitis
7) Pathergy test
Treatment modalities : It does not have any treatment. The symptoms can be treated by
i) Topical therapy -
a) Creams for the oral and genital ulcers
b) Eye drops for uveitis
ii) Systemic therapy -
a) Immunosuppressants like Infliximab.
b) High dose corticosteroids.
c) Colchicine can be used for genital ulcers but cannot be used here because of her G6PD deficiency.
iii) Cognitive Behavioural Therapy - which she is undergoing.